
Understanding the New Long-Term Data on Weight-Loss Drugs
Recent long-term research on GLP-1 medications has offered an unprecedented look at how these popular drugs perform when used for several years rather than months. Researchers followed participants over a four-year period and found that sustained use can help maintain weight loss far beyond what was previously documented. This new evidence highlights the chronic nature of obesity and reinforces the argument that long-term medical treatment may be necessary for many individuals. It also provides guidance for specialists who must evaluate whether medications should be continued indefinitely or as part of a structured plan. While the results are promising, they also reveal the importance of consistent monitoring, realistic expectations, and personalised care. Patients are encouraged to view these medications as part of a long-term strategy rather than a quick fix.
Sustained Weight Loss Requires Staying on the Medication

According to the OECD-The Organisation for Economic Co-operation and Development statistics from 2017, in the member countries, more than 1 in 2 adults and 1 in 6 children is overweight
One of the most important findings from the four-year research is that patients who continue the medication tend to maintain most of the weight they initially lost. Obesity specialists explain that this makes biological sense, since the body naturally works against weight loss through hunger signals and metabolic reduction. Long-term medication appears to counter those changes, allowing individuals to sustain progress without constant struggle. This differs significantly from traditional dieting, where regain is extremely common. The findings highlight that medications may need to be taken long term, similar to treatments for chronic conditions like hypertension. Patients should understand that discontinuing medication often leads to regain, not because the drug “stops working,” but because the underlying condition remains active. Long-term therapy therefore becomes part of a broader management plan rather than a temporary intervention.
Why Some Patients Discontinue Treatment Early
Despite the effectiveness of long-term treatment, not everyone continues for the full recommended duration. A meaningful share of patients stop due to side effects, most commonly nausea or digestive discomfort. Interestingly, the data suggests those with a lower BMI at the start of treatment are more likely to discontinue, even though side effects occur at similar rates across BMI categories. This raises important questions about personal tolerance, motivation, and perceived need for ongoing treatment. Some patients stop because they reach their target weight and assume continued treatment is unnecessary. Others may not fully understand the chronic nature of obesity and the risks of stopping too early. Healthcare providers emphasise the importance of explaining how long-term treatment works so patients can make informed decisions about continuation.
What We Know About Long-Term Side Effects

Ozempic is a prescription medication used for managing type 2 diabetes and is increasingly known for its off-label use in weight loss treatments.
While short-term side effects of GLP-1 medications are well documented, long-term side effects remain an area of active research. The four-year follow-up confirms that gastrointestinal issues typically occur early and may lessen with time. However, experts are still evaluating potential effects on gallbladder function, pancreatic activity, and long-term metabolic changes. Because obesity itself carries significant health risks, the benefits of sustaining weight loss often outweigh these uncertainties, but continuing medical supervision is essential. Blood tests, symptom tracking, and lifestyle monitoring help ensure safe use over many years. This long-term monitoring is especially important for patients who begin treatment abroad, as they will need consistent follow-up with a domestic provider once they return home.
What Happens When You Stop Long-Term Medication
The most consistent pattern across all research is that stopping medication typically results in weight regain. This does not mean the drug was ineffective; rather, it highlights obesity’s chronic and recurrent nature. Appetite tends to increase after stopping medication, and metabolic advantages diminish. Patients should be prepared for this possibility and discuss discontinuation plans with their healthcare provider. Some individuals may transition to lower doses, while others may switch to maintenance plans involving lifestyle-focused interventions. A structured discontinuation strategy can help minimise regain, but complete prevention is unlikely for most people. Understanding this reality helps patients set realistic expectations before starting therapy.
Why Long-Term Results Matter for Treatment Abroad
Weight-loss medications are increasingly part of international medical travel, especially for patients seeking metabolic evaluation or access to more affordable treatment. When starting therapy abroad, patients must consider what long-term follow-up will look like once they return home. Medication continuity, laboratory tests, and ongoing monitoring are essential for safe long-term use. Travel insurance does not typically cover long-term medication needs, so choosing appropriate coverage is important. Products described as medical travel shield or medical shield may provide some protection, but patients should confirm whether chronic treatment is included. Reliable international clinics will provide documentation and referral letters to support follow-up in the patient’s home country. This helps ensure continuity and reduces the risks associated with transitions in care.

Think your holiday insurance covers surgery abroad? Think again — learn why medical travel insurance is different.
Cost and Accessibility Over the Long Term
The high cost of semaglutide-based drugs is a major factor influencing long-term use. While some patients achieve life-changing results, the monthly cost remains a barrier. The new research highlights that stopping due to cost, rather than medical need, may undermine years of progress. Patients must evaluate whether long-term treatment is financially feasible and plan accordingly. Some individuals seek treatment abroad due to lower medication costs or more accessible prescribing frameworks, but they must account for additional expenses such as follow-up visits or travel. A transparent cost plan helps patients avoid unexpected interruptions that could affect long-term outcomes. Healthcare providers encourage discussing both financial and medical aspects before starting therapy.
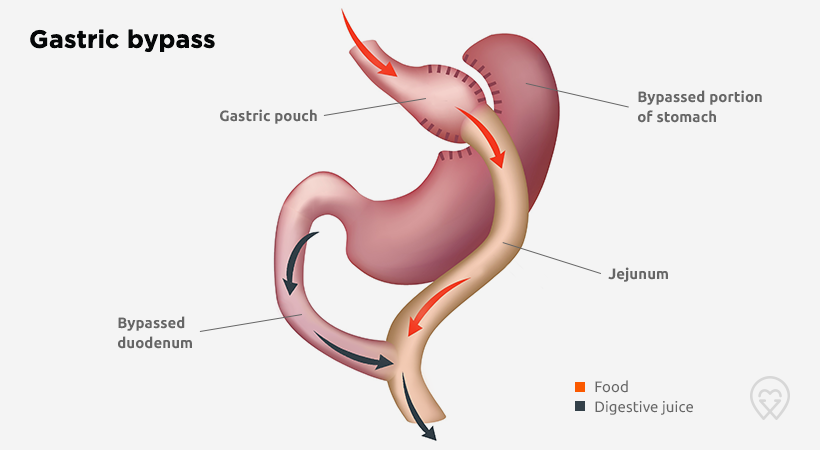
Comparing Long-Term Medication to Bariatric Surgery
Lower costs and shorter waiting times make bariatric surgery abroad an attractive option.
The four-year findings also influence how specialists view medication in relation to bariatric surgery. Bariatric procedures remain the most effective intervention for severe obesity, often providing the greatest total weight loss and metabolic improvement. However, long-term medication offers an option for patients who are not ready for surgery or who do not qualify based on BMI or health status. Some bariatric patients benefit from medication as a supplement if they experience partial regain. Specialists increasingly view surgery and medication as complementary tools, each with strengths for different patient groups. Patients should consult with qualified bariatric specialists to understand which approach aligns with their long-term goals and medical needs. Both options require continuing support, behavioural changes, and realistic expectations.
The Importance of Monitoring and After-Care
Long-term success with weight-loss medication relies on structured follow-up. Regular check-ups allow clinicians to monitor liver function, kidney performance, vitamin levels, and metabolic markers. Patients are also encouraged to track appetite changes, mood shifts, and lifestyle habits. After-care is especially important for those who initiate treatment abroad, as coordination between foreign and home-based providers ensures safe continuity. Clinics should provide written treatment plans, dosage guidance, and clear recommendations for follow-up intervals. Coordinated monitoring reduces risks, improves results, and allows for early detection of potential side effects. It also helps patients maintain motivation and adjust their lifestyle practices as needed.
Lifestyle Still Matters Even With Medication
Although medication plays a major role, lifestyle interventions remain essential. Diet, movement, sleep, and stress management all influence long-term success. Specialists emphasise that medication should not replace these factors but instead support them. Long-term treatment is most effective when combined with sustainable lifestyle patterns rather than strict dieting cycles. Patients who develop strong habits are more likely to maintain progress even if medication is adjusted later. International clinics offering treatment abroad often provide lifestyle guidance as part of the package, helping patients make long-term changes that travel with them once they return home.
Travel and Medication Continuity

Poland and Turkey are very popular destinations for bariatric surgery patients. The main reasons for this are the prices and high quality of treatment
Travelling while using GLP-1 medications requires planning. Patients should carry prescriptions, understand airline rules, and prepare for differences in availability between countries. Those receiving treatment abroad should confirm whether their home country will honour the prescription or require re-evaluation. Medication availability also varies, so patients should avoid relying solely on foreign supply chains. Insurance policies may not cover medical issues arising from treatment interruptions, making planning even more important. Clinics that specialise in treating international patients typically guide individuals through the necessary steps to ensure continuity before and after travel.
Summary: What Long-Term Research Means for Patients
The latest research marks a major step in understanding how weight-loss medication functions when used for years rather than months. Patients who stay on treatment tend to maintain weight loss, experience improved health outcomes, and enjoy better quality of life. However, long-term therapy requires ongoing monitoring, financial planning, and personalised medical support. Those considering treatment abroad must plan for continuity of care and ensure appropriate insurance coverage. When integrated with lifestyle strategies and professional guidance, long-term medication provides a powerful tool in the modern management of obesity.
Do weight-loss drugs continue to work long term?
Yes, the latest research shows that GLP-1 medications maintain their effectiveness over several years when used consistently. Patients who remain on treatment typically sustain most of the weight they lost during the initial months.
What happens if I stop taking the medication?
Most people regain some weight after discontinuing treatment. This is due to the return of appetite signals and reduced metabolic support. Patients should discuss a tapering or transition plan with their doctor before stopping.
Are long-term side effects known?
While most side effects occur early, long-term effects are still being studied. Issues such as gallbladder concerns, gastrointestinal symptoms, and metabolic adjustments require ongoing monitoring from a healthcare professional.
Are weight-loss drugs an alternative to bariatric surgery?
They can be an option for those who do not qualify for surgery or prefer a non-surgical approach. However, bariatric surgery typically results in greater long-term weight loss. Some patients use medication in combination with surgery.
Why do some patients stop the medication early?
Individuals may discontinue due to side effects, cost, or a belief that they no longer need treatment. Lower BMI patients appear more likely to stop early, even when side effects occur at similar rates across BMI categories.
Can I start weight-loss treatment abroad?
Yes, many patients begin treatment abroad, but continuity is essential. You must arrange for follow-up care, prescription access, and monitoring once you return home to ensure long-term safety.
Will travel insurance cover weight-loss medication issues?
Most standard travel insurance will not. Patients may need specialised plans, sometimes referred to as medical travel shield or medical shield, depending on the clinic or provider. Always verify coverage in advance.
Is long-term monitoring necessary?
Yes, regular follow-up appointments help assess metabolic health, organ function, and treatment effects. Long-term use of GLP-1 medication requires medical supervision.
How often will I need check-ups?
Most specialists recommend check-ups every three to six months, but this may vary depending on your health profile, dosage, and any existing medical conditions.
Can lifestyle changes reduce my need for long-term medication?
Lifestyle strategies are essential and can improve results, but most patients see the best outcomes when combining medication with diet, movement, sleep, and behavioural support. Medication alone is rarely sufficient for lasting success.
-
Wilding J.P.H. et al. “Once-Weekly Semaglutide in Adults with Overweight or Obesity.” The New England Journal of Medicine.
-
Rubino D. et al. “Effect of Continued Weekly Subcutaneous Semaglutide on Weight Loss Maintenance.” Diabetes, Obesity and Metabolism.
-
STEP Program Clinical Trials (Semaglutide Treatment Effect in People with Obesity) — Multi-year data summaries published via NEJM and Diabetes Care.
-
American Society for Metabolic and Bariatric Surgery (ASMBS). “Guidelines and Indications for Obesity Treatment.”
-
National Institute for Health and Care Excellence (NICE). “Semaglutide for Managing Overweight and Obesity.”
-
World Obesity Federation. “Chronic Obesity Management and Pharmacotherapy Guidelines.”
-
U.S. Food and Drug Administration (FDA). “Safety and Regulatory Information for GLP-1 Receptor Agonists.”



