
Revenue Cycle Management (RCM) is an essential part of a well-functioning healthcare system. The financial processes running in the background handle payments to providers, allowing medical teams to devote their time and energy to patient care. A good revenue cycle is important for the financial stability of healthcare organizations, even if they are well-run.
As the industry becomes increasingly complex, the management of healthcare revenue has emerged as a strategic priority. The entire process—from registration to final payment—must be accurate, timely, and compliant with regulations. P3Care, for example, provides significant support to companies in revenue cycle management, ensuring no revenue is missed and that each claim is processed accurately.
What Revenue Cycle Management Really Involves
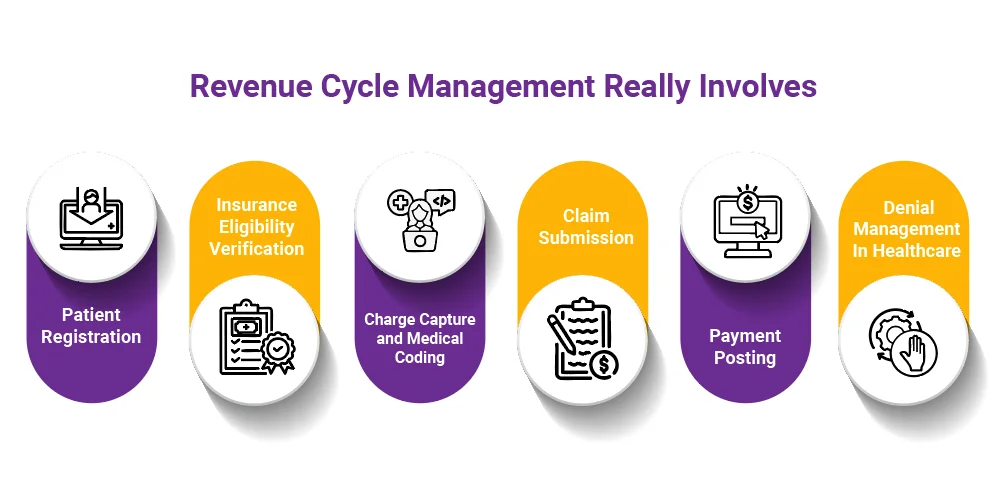
RCM comprises several linked stages that span from the time a patient books an appointment to the moment the provider receives full payment. The stages consist of:
- Patient registration
- Insurance eligibility verification
- Charge capture and medical coding
- Claim submission
- Payment posting
- Denial management in healthcare
The success of the entire healthcare reimbursement process depends on every step, and even a single mistake can lead to payment delays or denials, resulting in significant losses.
Why Revenue Cycle Management Matters So Much

1. Faster, More Accurate Reimbursement
Revenue Cycle Management (RCM) is responsible for filing claims properly the first time around. Clean claim approvals lead to fewer reworks, faster payments, and no delays, helping providers maintain stable cash flow.
2. Stronger Financial Health
A successful revenue cycle results in fewer mistakes, fewer documents processed, and more easily predictable income. Such a scenario attracts healthcare organizations willing to invest in advanced technology, patient care, and human resources.
3. Fewer Denials and Less Revenue Loss
Claim payment denials continue to pose a major financial challenge for hospitals and clinics. Well-grounded denial management in the healthcare sector recognizes the root causes of issues early, thereby preventing future revenue leakage and strengthening the organization’s financial performance.
4. Better Patient Experience
A patient’s impression of the healthcare environment will depend on how transparent the billing process was, the accuracy of the insurance verification, and the communication that took place. A solid revenue cycle plays a crucial role in patient satisfaction as much as the medical treatment provided.
5. Compliance and Risk Reduction
RCM serves as the police of payer rules, along with documentation standards and regulations, while also serving as a shield for providers against penalties and operational risks.
Revenue Cycle Optimization: A Key to Better Performance
Optimizing the revenue cycle leads to:
- Better clean-claim rates
- More efficient workflows
- Improved financial reporting
- Reduced administrative overhead
Well-organized procedures and a robust control system enable firms to handle daily operations and complex billing issues more efficiently. Many of them seek professional help from companies such as P3Care to achieve greater transparency, fewer errors, and a more efficient revenue cycle.
Challenges in Healthcare Revenue Management
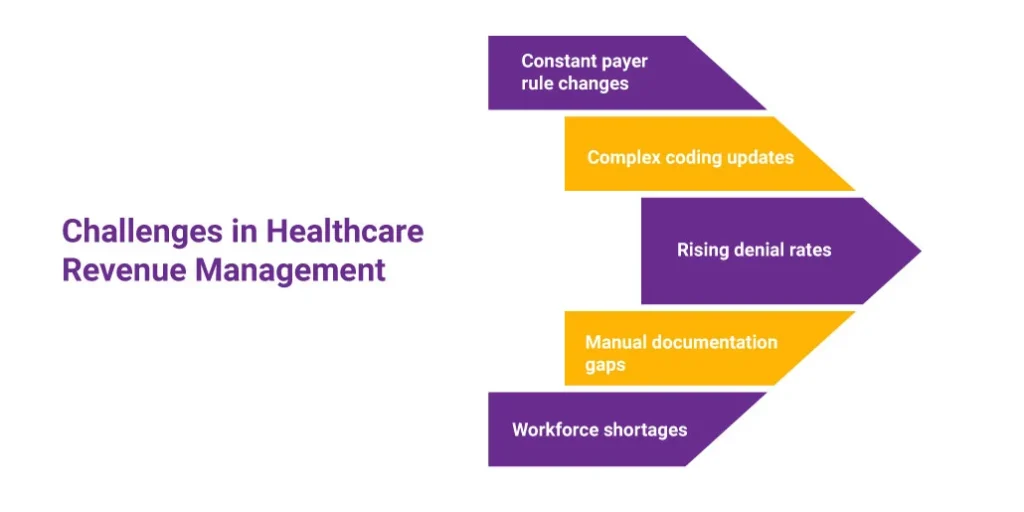
Even with good systems, the revenue cycle faces ongoing challenges, such as:
- Constant payer rule changes
- Complex coding updates
- Rising denial rates
- Manual documentation gaps
- Workforce shortages
Recognizing these challenges makes it easier for organizations to refine their healthcare revenue management strategy.
How Technology Enhances the RCM Process
The technology is responsible for the big changes RCM is undergoing. The combination of automated eligibility checks, AI-assisted claim entry, and billing platform integration is key to identifying errors early and reducing manual work. And predictive analytics provides teams with real-time insights into denial patterns and payment trends. The accuracy and transparency in the workflow have been improved to such an extent that the RCM process is now quicker and more trustworthy.
Conclusion
Revenue Cycle Management is the main pillar of financial soundness in the healthcare industry. The smooth running of the revenue cycle results in timely payments to providers, clear information for patients, and a confident stance for organizations. With the assistance of reliable, experienced partners like P3Care, healthcare providers can refine their RCM processes and remain focused on ensuring the quality of care.
Frequently Asked Question
1. What is revenue cycle management in healthcare?
RCM is an all-encompassing process that handles every administrative and financial task from patient registration through final payment, ensuring accurate billing and on-time reimbursement.
2. Why is RCM important for healthcare providers?
RCM ensures that a healthcare business remains financially stable, minimizes errors, accelerates payments, and improves patient communication and support.
3. What causes most claim denials?
The most frequent reasons for denials are coding errors, missing documentation, patient eligibility issues, and incomplete information in the claim.
4. How does revenue cycle optimization help?
It helps by making operations more efficient, increasing the rate of clean claims, reducing delays, and boosting the healthcare provider’s financial performance.
5. How does RCM improve the patient experience?
Patients are kept informed and experience less financial stress due to clear billing, accurate verification of insurance coverage, and timely updates.
6. Can outsourcing RCM benefit healthcare organizations?
Many organizations are working with specialists like P3Care to reduce administrative burden and improve billing accuracy.






